Think about synergy between medicine and basic sciences.This collaboration is necessary to achieve the digital shift of the medical sector, that is smart health and natural!
For this, it is necessary to integrate in the medical sector certain principles already used in the three economic sectors, including very largely in the tertiary sector to which the services to the person belong. I am thinking of the use of equivalent techniques of consumer relationship management, and other sophisticated uses of datas, chatbot and blockchain techniques …
It must be said that the medical sector is a very special sub-sector of the tertiary sector. It seems more impervious to cultural developments that impact society as a whole.
There is a paradoxical side between the rapid evolution of medical knowledge and the very conservative character of doctors sociologically.
Indeed medical excellence can be expressed by the half-life of medical knowledge (half-time obsolescence of a major issue review in a medical discipline). It continues to shrink and has dropped below the 5 and a half year mark
The vast majority of doctors are used to constantly listening to progress, and continuing professional training is rather well organized (validation of training by ANDPC, role of OPCAs). for employees). The supervision of this postgraduate training seems to make progress even if much is left to the free will of health professionals. Accreditation of physicians who belong to specialties at risk is encouraged but not required. The Continuous Professional Development approach is mandatory but to my knowledge, there is no significant control.
Despite these remarks, it is clear that health professionals have acquired since their student path this culture of permanent challenge to knowledge.
But if this is true for the heart of their medical activity, it is not at all the same with respect to the organization of the profession and communication.
Health professionals and doctors in particular are adopting very slowly, and often under duress, new operating techniques.
Even today financial aid is offered to doctors for;
– Keeping the computerized medical file with clinical data entry allowing individual and patient follow-up.
– The use of certified prescription assistance software or non-prescribing physicians (PCA) of a standardized reporting module.
Computerization makes it possible to teletransmit and use teleservices
With the incentives, in 2009 still more than 32% of the invoices of the doctors (leaves of care) were carried out using sheets of care paper, which corresponded to more than 110 million sheets over one year.
The prerequisite for truly initiating the digital transition of the medical sector is the generalization:
-Doc Shared Medical Record (DMP) with interoperability with the computerized patient record of practices and care institutions, (note that currently in the liberal sector, there is not in fact interoperability between patient files of cabinets and MCO establishments for example).
– the use of encrypted messaging (MS health, Apicrypt) for the transmission of medical documents between doctors.
– the dematerialization of medical prescriptions made available directly to the patient or the pharmacy.
In fact, it would require a single data base, ie a universal medical record that can be used by all: patients, city and hospital doctors. In this regard, only private initiatives seem to be promising; For example, the Passcare, a true medical passport that can accompany a patient worldwide with chronic diseases and can provide optimal care anywhere in the world.
we have long been campaigning for the idea of a universal, unique, ideal application, which should include:
– The patient’s medical file. In this medical file as we dream, the patient should be able to register everything he wants. He should be able to find all the data of his consultations with his referring GP, the data provided by his specialist doctors, the letters exchanged between these different doctors, including the letters between the hospital and the city doctors. All radiological, biological, anatomopathological examinations …. With the reports, or even the comments and the follow-up of its medical prescriptions, the medicines delivered by the pharmacies.
– Would be integrated in this digital file of “dream” all the necessary modules to help him manage:
-A surgical intervention, with a file “course of care” adapted to each intervention and gathering all the information concerning the pre, the per, and the postoperative (immediate and long course).
– A chronic disease, with a diabetes module, adapted oncology, cardiovascular diseases (coronary heart disease, heart failure), renal failure, psychiatric pathology and cognitive disorders (accessible and affordable by caregivers), dysthyroidism, morbid obesity, HIV ……
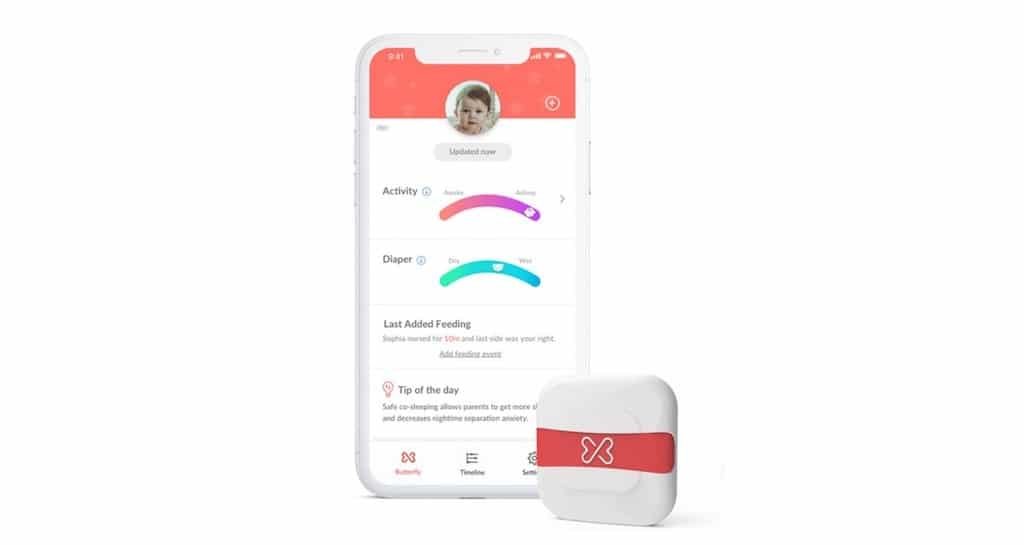
– But perhaps the most important would be the integration of a fundamental module dedicated to prevention, device by device, with advice on healthy living and advice to use modern means of self-monitoring. This module should be the most ambitious, the most complete possible, it should eventually allow to use as little as possible other “therapeutic” modules that too often sign the failures of health policies or precisely prevention is the poor relation.
But such a tool does not exist.
What can be done about this impossibility of ordering and coordinating patient data?
This is where the data-scientist and engineering mathematicians must intervene … They must create digital systems that will imitate what we already knew how to do by direct speech, by replacing the paper, the telephone, the SMS, the mail ….
It’s up to them to invent new solutions thanks to new mathematics and new computers that will feed on the medical data that we clinicians will need to learn to order.
It is the private initiatives that will bring us solutions.
What will cheer us up is the work of ant between doctors and engineers and other specialists in digital marketing that will hatch new APPs.
One of the best examples of collaboration between medical research and the new basic sciences is represented by London-based BenevolentAI.
The two divisions of Benevolent work not side by side but together, showing this singularity of combining I.A. to medical research.
This is very emblematic of the nascent affirmation of the synergy between NICTs (here new mathematics, new computers …) and the industrial world (here medical). Ken Mulvany, founder of BenevolentAI, says today, “BenevolentAI technology can identify correlations that a human researcher would never think of looking at.” Researchers can also use I.A systems. to analyze a disease. Allowing them to state new assumptions previously impossible, because of the amount of data that artificial intelligence can handle. BenevolentAI thus has drugs in development.
Medicine will thus be able to respond more favorably to the expectations of the public who want a better organization and a better effectiveness of the care and especially a better taking into account of the prevention.
Click here to read more about smart health
Summary article Advocacy for the synergy between medicine and basic sciences from :
http://innovationesante.fr/plaidoyer-pour-la-synergie-entre-medecine-et-sciences-fondamentales/